Things have been a little rough, but I’m turning them around.
As it turns out, going through the Stages of Grief on steroids during the holidays with your family around is the recipe for a horrible nightmare.
Or at least pretty serious depression. But who can tell, with the steroids?

Might be less stressful for everyone involved.

Seriously.
But, the holidays are over now and I’ve reached Acceptance (again, for now) and I go back to work tomorrow and I’m feeling a lot better. For now. Until my next mood swing. Or spot of bad news.
I’ve done a lot of research into my disease this week. It started as research into an alternative diagnosis, spurred on by a few things:
- Everyone keeps talking about how “very unique” my case is.
- IgA Nephropathy is a very dissatisfying diagnosis — cause is unknown and it’s a bit of a catch-all.
- IgAN is not a something I want to have — it has no cure, known treatments are basically 50/50, and it could recur even if I get a kidney transplant.
So, I went hunting for a new diagnosis. It seemed promising at first. All of the American scholarship around kidney disease is typical American bullshit — focuses exclusively on old white guys with kidney disease, skewing all of our data. In America, we don’t even really bother screening for kidney problems until it’s way too late, lest we give people an opportunity to actually adjust their lifestyle and not kill themselves with sodium overload and a high-protein diet. It’s so fucking stupid. In Asia, they screen young people regularly for early signs of kidney problems, which tons of people have, so they change their diet and repair their kidneys and live longer without chronic kidney disease. The fact is we’ve just accepted that the kidneys degenerate over someone’s lifespan and have decided to not really do anything about it and then just blame it on high blood pressure or diabetes when it becomes a problem when people are 70. The problem I’m having is something has caused my kidneys to degenerate extremely fast 40 years early and no one call tell me what that is, which is exceptionally frustrating. I didn’t suffer an injury to my kidney, I’m not diabetic, and it’s unlikely I had high blood pressure before my kidneys were damaged. So what caused this?
I went looking for cases of kidney disease in other young people in other parts of the world. I was able to dig up that dehydration is most certainly a factor — kidney disease is killing young farm workers in Central America and India at alarmingly high rates. Unfortunately, I have about as much in common with young farm workers as I do with someone who’s 70, so this information is of limited use to me. I did discover that what’s happened to me is starting to happen to more young Americans, and also younger people in urban India. There’s certainly a lifestyle component, but that alone doesn’t explain what’s happened to me — otherwise everyone my age would be in kidney failure. High blood pressure is a red herring. It comes with the kidney failure. If I had HBP long enough to cause kidney damage I would see damage in other organs as well, which I don’t.
I live a substantially healthier lifestyle than the average person my age, so the only thing that actually makes sense is that something totally stupid and random like igAN would happen to me. I’ve been doing a lot of things right since college — my vegetarian diet is already lower protein than most people’s and much closer to the recommended. I had already been making efforts to reduce sodium. I was already avoiding things like transfats and high-fructose corn syrup and refined sugars and other additives and flavorings and things that aren’t actually F O O D. I made all of these changes 7-8 years ago. The only thing I could have really done better is eat less cheese. I could have been exercising more, but I walk a fucking ton, more than enough to keep healthy. Healthier than average. Healthy enough to avoid fucking major organ failure. I’ve already been drinking less alcohol the last few years than I was before. I’ve limited my coffee to one strong one a day (most days) for the last five years. I’M A HEALTHY FUCKING PERSON. Which I’ve had confirmed, aside from my kidneys, all of other organs are in tip-top shape, including my heart and my liver which are now at the greatest risk. My blood sugar is great. My cholesterol is normal. It’s really frustrating to be googling lifestyle changes to help my kidneys and find a list of shit I’ve already been doing for 8 years. Salt being bad for you is not fucking news to me. I guess I’ll eat less cheese and chocolate. I’ve already cut out alcohol and caffeine.
So, I took the long way around, but ended up validating the igAN diagnosis.
A disease of the kidney, specifically a form of glomerulonephritis: an inflammation of the glomeruli of the kidney.
“Very rarely (5% each), the presenting history is:
The proteinuria and cutaneous edema characteristic of nephrotic syndrome are my two main kidney disease symptoms — they’re the ones I had leading up to my hospital stay and the ones I still have now that my kidney function hasn’t improved. Plus the hypertension and anemia I presented with, but don’t have anymore. My anemia is nearly cured, maybe, and my hypertension is managed with meds for now. I get other kidney symptoms; flank pain, so far only on my left side, as punishment for not following my diet well enough and straining my kidneys; and still fatigue. Everything else I’m dealing with is side effects from treatments, or issues related to my pH/electrolyte/nutritional imbalances due to kidney failure, which are mostly managed with meds. For example, my calcium absorption is all fucked up, plus the steroids are actively trying to wreck all my bones. I’m at risk for hypocalcemia, so I’m taking a ton of calcium supplements everyday, but if my eating schedule gets weird, or I forget to take them, or I take them to close to food or other meds that block absorption, I don’t get enough calcium, and I get tremors (which could also be from the steroids, or just fatigue), or if I do this badly for over a day, I get cramps in my hands and feet. My left hand, in particular, making it really hard to use. So, it’s a fun trade off. I can eat cheese and insure I get enough calcium, but I’ll know I’m straining my kidneys when my back/side starts fucking killing me; or I can not eat cheese (be miserable) and be hyper-vigilant about my calcium absorption otherwise my left hand freaks out while I’m trying to drive somewhere.
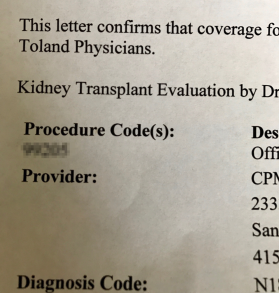
Now that I’ve settled into my diagnosis, shitty as it is, I feel more proactive again. I’ve doubled down on research into my disease. Josh has thrown all the available conventional treatments at me already, and there’s basically only a 50% chance they’ll have any positive effect. The best case really just postpones the inevitable — Stage 5 kidney failure. Stage 5 means dialysis and kidney transplant if I want to live, so postponing that is good. My numbers are already technically Stage 5 numbers, but I’m still symptomatic of Stage 4, which is good, but not comforting in the slightest. Finding a living donor kidney and setting up my Backup Plan is still Priority 1. (Has been difficult to get any traction during the holidays — the transplant program office has been closed for non-emergencies.) Transplant comes with a ton of new bullshit and it won’t cure my igAN, so I’m probably looking at immunosuppressants for the rest of life, which is really really depressing. So we’re just going to not think about that now because there’s nothing we can do about it and it launches me into a pit of despair which I already cried about for like five straight days.
What I can do something about is my diet, which I’ve been led astray on a bit. I should definitely continue being vegetarian. A low-potassium vegetable-based diet is the best thing for my kidneys, not to mention the rest of my body. There’s too much protein and phosphorous in most dairy, so I’ll be limiting those more strictly as well. This makes me feel better. Onions, red bell peppers, garlic, parsley, and apples are my kidney superfoods and I’m going to eat them everyday. Over the Christmas weekend I ate way too much cheese and chocolate and I super paid the price for it — I had persistent flank pain for days, some of the worst fatigue since the first few days after leaving the hospital, headaches (not migraines), and just the most depressive fucking mood. First I blamed what I assumed (hoped?) was low blood levels from my chemo nadir, but labs came back and my blood levels were up, so that wasn’t it. Then I ate just vegetables for two days and felt better. Vegetables are the best.
Because my blood levels were so good the other day I didn’t get my hormone boost, so now we’re experimenting to see if they go down without it or if I’m not anemic anymore. The phrasing the nurse practitioner used was “it’s a little risky — hopefully in a week we don’t see you circling the drain“. That seemed a little indelicate, for someone I had just met, even by my standards. But anyway, it’s almost a week later and I still feel pretty good. I have chemo next week, so we’ll find out then. It took me a week to lose the 8lbs I gained from chemo last time, so looking forward to that again. Right now I’m down to 123lbs, which is nearly what I was before I went into the hospital, so normal. I’m still Staypuft from the prednisone, but less Sausage D in general. I’m not due to see Josh for another 3 weeks, but I think I need to get him on the phone sooner, because we should be tapering my prednisone sooner than that if we can. I finally had my follow-up with my PCP last week. Last time I saw her was the day we met and she immediately identified I was in kidney failure and threw me at Josh, so obviously a lot has happened since then. I was still in a pretty fucked up emotional state when I saw her. She offered to refer me to a therapist.
I get a week of normalcy this week, which I’ll need because work is going to be crazy. Getting through it with my prednisone mood swings is probably all I can fit on my plate.